
Filmed November 2021 – edited into 10 parts; total 170 minutes
Download the presentation handout (71 pages)
Many children and adolescents with autism and other neurodiverse conditions present significant concerns to carers who are trying to ensure proper levels of nutrition. This presentation begins with a discussion of selective eating and the factors that can affect a child’s eating. Our presenters then discuss how food preferences develop and the importance of children tasting a wide range of foods.
Step by step strategies for expanding a child’s diet are included, such as ways to increase the likelihood your child will take a bite, and how to respond when your child is refusing.
The presenters provide answers to questions commonly asked by parents during therapy, including:
- “What if I’ve tried rewards but my child still won’t take a bite?”
- “Will my child always rely on rewards to eat new healthy foods?”
- “What if it never gets easier to feed my child?”
- “When do I honour my child’s dislike for a new food?”
- “What if my child is sensitive to textures?”

About the Presenters
Lauren Binnendyk, PhD, BCBA-D
Lauren Binnendyk has a PhD in Special Education (concentration in autism and related disabilities) and is a Board Certified Behavior Analyst (BCBA-D) and has worked with children with developmental disabilities since 1997. Dr. Binnendyk is the Clinical Director at West Coast Feeding and Behaviour Specialists which she opened in 2010 to provide families with evidenced-based, family centred treatment of severe feeding disorders. Her practice has expanded to include a range of feeding concerns including, picky eating, bottle or milk dependence, chewing issues, and Avoidant/Restrictive Food Intake Disorder (ARFID).
Chantal Juilfs, M.Ed. BCBA, Behavior Analyst Consultant
Chantal received her Master’s degree in Special Education (concentration in developmental disabilities) from the University of British Columbia in 2017 and is a Board Certified Behaviour Analyst. In 2013, Chantal began specializing in feeding disorders under the supervision of Dr. Binnendyk at West Coast Feeding and Behaviour Specialists. Chantal has focussed her practice on working with individuals diagnosed with Avoidant Restrictive Food Intake Disorder, food selectivity, food refusal, and oral motor delays. Chantal understands the underlying fear involved with trying new foods for most of the individuals she works with and uses evidenced-based strategies to help them work through their fears to reach their goals.
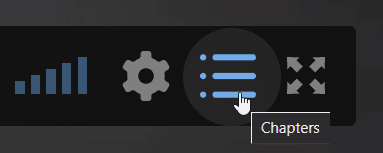
New feature on Autism Videos @ ACT
Navigate videos with “chapters”
Chapters help you navigate through a video to find the information you’re looking for. Click the blue dots on the timeline to navigate chapters, or see all chapters through the chapters icon on the bottom right of each video.
Part 1: Introduction
Part 2: Avoidance Restrictive Food Intake Disorder (ARFID)
Part 3: How do I Expand my Child’s Diet? – Taste Exposures
Part 4: Antecedent Strategies
Part 5: Consequence Strategies
Part 6: Case Study #1: A 5-Year-Old with Selectivity & Rigidity Feeding Issues
- 5 years old at the start of intervention
- Lives with his parents – with grandparents from after school until dinner time
- Diagnosed with ASD
- Feeding Issue: Selectivity, rigidity
- Mealtimes: EL had a typical eating routine until he went with his dad to visit family in another province for a week. EL started to drop foods quickly until he had 4 in each food group, and many foods that were “hit/miss” and started only eating a few bites of the foods on his accepted food list.
Part 7: Case Study #2: A 20-Month-Old with Anemia & Selective Feeding Issues
- 20 months old at the start of intervention
- Lives at home with her parents
- Background:
- Born with a heart defect and underwent surgery after birth
- Diagnosis of ASD
- Feeding issues:
- Has always been a picky eater
- History of eating a food for 1‐2 weeks and then dropping it.
- Anemic
- Mealtimes:
- Sits in a high chair or stands on a learning tower
- Eats completely distracted
- Breastfed throughout the day
Part 8: Case Study #3: A 3-Year-Old with Oral Motor Delays & Selectivity Feeding Issues
- 3 years old at the start of intervention
- Lives with his parents and two younger brothers
- Diagnosed with ASD
- Feeding Issue: Oral Motor Delays & Selectivity
- Round 1: Purees
- Round 2: Chewing Intervention
- Round 3: Variety, Speed, and Chewing
- Mealtimes: Ate mealtimes with family, but highly selective with new foods. If he accepted bites of non‐preferred foods, he would pack them in his cheek pocket for hours.
Part 9: Before You Start Tasting Sessions/Common Mistakes and Questions
Part 10: Q and A
Use the chapters menu on the bottom right of the video to see the list of questions.
00:00 – Different experiences for different children?
1:10 – Siblings for peer modeling?
2:01 – Who diagnosis ARFID?
2:31 – Dealing with older children?
3:58 – Hungry vs. Hangry?
5:00 – Grossed out by other people eating?
6:44 – Reinforcement and rewards?
8:32 – Pathological demand avoidance and food?
9:20 – Tolerance overall?

